
Rebecca Ryan BMBS (Hons) FRACP
Endocuff Techonology now being offered to patietns at all Montserrat Facilites across Queensland
One of the major indications for colonoscopy is for Polyp follow up or for a Family history of Colorectal carcinoma/colonic polyps.
Performance of a high quality colonoscopy examination requires careful visualisation of the colonic mucosa which requires
1/ Adequate Bowel Preparation
“Split bowel preps” refers to the administration of half of the bowel prep the evening prior to the colonoscopy and the second half the morning of the colonoscopy, allowing for adequate fasting .
Since the introduction of split bowel preps at Montserrat in (insert date here) our rate of incomplete colonoscopies due to poor/incomplete bowel preparation has (insert data).
2/ Quality Measures
Quality indicators such as
- Acceptable caecal intubation rate,
- At least 95% to the caecum or terminal ileum in patients with intact colons.
- Withdrawal times
- Should be 6 minutes (not including biopsy or polyp removal time)
- Adenoma detection rates (ADR)
- The finding of at least one adenoma during colonoscopy
- At least 25% in eligible patients.
“Eligible patients” are 50 years or older, have intact colons, do not have a finding of acute IBD and were intubated to the caecum or terminal ileum.
serve as surrogate, though imperfect markers of careful mucosal visualisation. These targets have been set by GESA (Gastroenterological Society of Australia for re-certification of colonoscopists in Australia) as of April 2016.
At Montserrat we routinely record all our procedures, a selection of which are routinely audited by a independent senior experienced colonoscopist. We also document our caecal intubation rate, withdrawal time and ADR, for all our gastroenterologists to ensure we are meeting the above targets. These are viewed and discussed quarterly at our quality assurance meetings.
Despite implementation of these measures, we know we miss adenomas.
6 studies of 465 patients who underwent tandem colonoscopy showed
The overall missed adenoma rate was 22%and proportional to size (Ref 1)
- 1 to 5 mm: 26 percent miss rate
- 5 to 10 mm: 13 percent miss rate
- ≥10 mm: 2 percent miss rate
Higher ADR has been demonstrated in multiple studies to decrease the rates of interval cancers (ie, cancer that developed between the time of the screening colonoscopy and the time scheduled for follow-up colonoscopy)
In a study of 45,026 patients who underwent screening colonoscopy, interval colorectal cancer (ie, cancer that developed between the time of the screening colonoscopy and the time scheduled for follow-up colonoscopy) was detected in 42 patients. (Ref 2)
The endoscopists’ adenoma detection rates were associated with the risk of developing an interval colorectal cancer. The rates of interval colorectal cancer were
- 34 per 100,000 person-years for endoscopists with an ADR <11%,
- 22 per 100,000 person-years for endoscopists with an ADR 11 – 14.9 %
- 26 per 100,000 person-years for endoscopists with an ADR of 15 -19.9 %,
- 2 per 100,000 person-years for endoscopists with an ADR ≥20 percent.
In another study, each 1% increase in the ADR was associated with a 3% decrease in the risk of colorectal cancer. Ref 3
How can we increase the Adenoma Detetion Rate (ADR)?
ENDOCUFF VISION ®
Put in pretty picture and link to online brochure
Endocuff Vision ® is a ‘cap’ designed to fit securely around the tip of the colonsocope and is comprised of soft projection s (arms) which remain flattened during insertion in the bowel. When the colonoscope is withdrawn the soft arms project out to spread the folds of the colon. This allows for improved visibility of the bowel wall and more opportunity to find hidden or harder to see polyps.
In observational studies to date ENDOCUFF VISION ® has been shown to
Increase ADR
Increase mean number of Adenomas per procedure
Relative decrease in the mean time to caecal intubation Ref 3
Montserrat will be, as of (insert date), routinely using ENDOCUFF VISION ® in ALL patients that are
- over the age of 50
- Have a personal or family history or polyps or CRC.
Don’t know if you ant to put in the that we are absorbing the cost etc.)
Ref 1
Polyp miss rate determined by tandem colonoscopy: a systematic review. van Rijn JC, Reitsma JB, Stoker J, Bossuyt PM, van Deventer SJ, Dekker E, Am J Gastroenterol. 2006;101(2):343.
Ref 2
Quality indicators for colonoscopy and the risk of interval cancer. Kaminski MF, Regula J, Kraszewska E, Polkowski M, Wojciechowska U, Didkowska J, Zwierko M, Rupinski M, Nowacki MP, Butruk E, N Engl J Med. 2010;362(19):1795.
Ref 3
Tsiamouulos Z, et al. gastrointestinal Endoscopy 2015; 81 (5s): AB209 Abstract Sa 1423




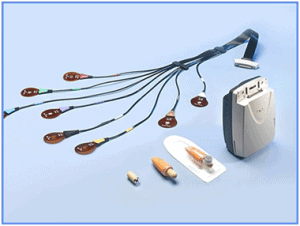 Since its introduction in 2000, capsule endoscopy has allowed us to investigate and diagnose pathology in the small intestine, a previously arcane area of the gastrointestinal tract.
Since its introduction in 2000, capsule endoscopy has allowed us to investigate and diagnose pathology in the small intestine, a previously arcane area of the gastrointestinal tract.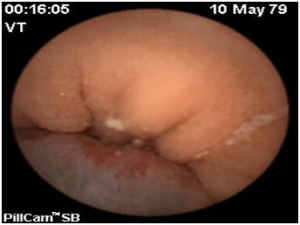 Capsule endoscopy has a sensitivity of 47% and 66.6% respectively for the detection of pathology in occult bleeding or iron deficiency anaemia. Where pathology is detected, the patient may then need to be referred for enteroscopy to obtain a tissue diagnosis or for interventional procedures.
Capsule endoscopy has a sensitivity of 47% and 66.6% respectively for the detection of pathology in occult bleeding or iron deficiency anaemia. Where pathology is detected, the patient may then need to be referred for enteroscopy to obtain a tissue diagnosis or for interventional procedures. Great effort to the Montserrat Cancer Care Team: The Full Montyserrat
Great effort to the Montserrat Cancer Care Team: The Full Montyserrat